Fascia: properties of fascia and tissue manipulation
One of the targets of manual therapies is to treat dysfunction of the body by working the fascia. In the previous post I wrote about fascia, I discussed its properties and its relation to muscles and organs.
Here I will write about how manual treatment can treat body dysfunction by altering the fascia properties.
I came across an interesting article on fascia plasticity written by Robert Schleip, director of the Fascia Research Group, Division of neurobiology at Ulm University in Germany. In his paper, Schleip suggests that change in fascia plasticity is not the result of a pure bio mechanical stress (tissue manipulation). He proposed a neurobiological explanation on how fascia can alter its own structures. But let’s start from the main concept.
The main concept is that manual treatment can alter fascia properties because fascia has the ability to adapt and change to physical stress (Rolf 1977, Chaitow 1980, barnes 1990, Paoletti 1998).
Two main theories have been advocated to explain this phenomenon: the Gel-to-sol model and the Piezoelectricity model.
The first one, advocated by Ida P. Rolf, states that fascia is a connective tissue of colloidal substance, which means made of a glue-like substance that changes it’s state from a more dense “gel” state to a more fluid “sol” state when it is moved (Rolf 1977). An example would be a dice of butter that is solid, and once heated it becomes liquid to then change again to solid state once it gets cold again. This property of the fascia is called thixotropy and occurs when mechanical stress, for example manual treatment, is applied to the connective tissue (Twomey & Taylor 1982). One of the main objections to this theory is that connective tissue is time and force dependent which means it needs long term and more force than normal tissue manipulation to get deformed. Some researches (Currier & Nelson 1992) have shown that manual treatment is unable to provide either the time or the force sufficient to modify fascia property in a short term.
The release felt by the practitioner is not probably related to the plasticity of the fascia itself but maybe to the muscle relaxation of the patient during the treatment. The other theory states that connective tissue has the same properties of a “liquid crystal” substance (Juhan 1987) that can be altered by pressure (Oshman 2000). The cells composing the connective tissue, called fibroblasts and fibroclasts, release electric charges due to mechanical pressure that can alter fascia plasticity. The objection to this theory is that the half-life span of connective tissue has been shown to be between 300 and 500 days, and the half-life of the matrix of the connective tissue is between 1.7 and 7 days (Cantu & Grodin 1992) which is well above the hour used to deliver a manual treatment.
The two previous models might explain the change of fascial connective tissue in a long term but not in a short term. The question here is: how can a practitioner change fascia properties in a session of manual treatment? Better: what is that feeling of release that either practitioner or patient feels during manual treatment?
A new theory has been advocated in light of research on fascia neural property (Cottingham 1985, Ward 1993, Schleip 1989). Fascia is said to be abundant in certain mechanoreceptors (nerve endings) like Golgi receptors which are sensitive to muscular contraction (Schleip 1989), Pacini and Paciniform receptors which are sensitive to vibration (Yahia et al 1992), Ruffuni receptors which are responsive to tangential force and lateral stretch (van den Berg & Capri 1999), and interstitial receptors which are susceptible to sustained pressure change (Mitchell & Schmidt 1977).
Also it has been discovered that in typical muscle nerve only 10 – 20% of neural fibres are dedicated to the motor component. The remaining 80 – 90% is used for the vasomotor and the sensory component (Engeln 1994).
This brings an important new concept: the change in temperature and fluid (blood supply) within a muscle or connective tissue during deep tissue treatment can explain in part the release felt by the practitioner and patient.
The interstitial mechanoreceptors also have been shown to have both mechanical function (activated by sustained pressure) and automonic function (change in arterial blood pressure, heart rate and respiration) (Coote & Perez-Gonzales 1970). Those actions can alter the chemical composition and the release of chemical substances used to relieve tension in muscles and fascia (Melzack & Wall 1965). Some studies have shown that an increase of static pressure on muscles tends to lower arterial blood pressure (Mitchell & Schmidt 1977) thus changing the tone of the surrounding soft tissue (relaxing and loosening sensation after deep tissue treatment).
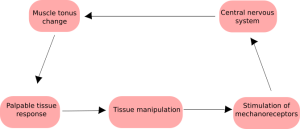
How tissue manipuation can change tissue thixotropy properties according to Cottingham central nervous system loop
The conclusion is that immediate fascial plasticity and releasing sensation felt by patient and practitioner cannot be understood by fascial mechanical properties alone. In light of the fact researchers found the existence of nerve endings in fascial tissues and their action within the fascial tissues a neurobiological explanation can better explain how the fascia works, and how deep tissue treatment can alter its properties in the short term.

